STIs Explained (Since Sex Ed Probably Didn't Teach You Enough)
If you grew up in the United States, there's a pretty good chance that your sex education was pretty limited, if you had any at all. In the U.S., sex education isn't federally mandated and isn't required in all states. However, comprehensive sex education is important to lifelong health and well-being. The curriculum goes beyond just sex and covers healthy relationships, boundaries, and consent, as well as details about STI/HIV prevention, testing, and how to navigate an STI diagnosis.
So, what has this lack of education done to us? It's given the U.S. an STI epidemic and one that, according to the Centers for Disease Control, isn't going to cease soon. Even with such a prevalence, there's a misguided belief that STIs are essentially obsolete. Harvard Medical School lecturer Whitney Irie tells The New York Times, "I don't think there's a clear understanding, especially among people with a uterus, of the long-term impact on your reproductive organs. There's this casualness about it that lends itself to being casual about preventive measures."
Since we obviously need a refresher on STIs or, in some cases, an introduction, here you go: STI 101.
Condoms don't prevent STIs
Although, yes, latex condoms can prevent HIV and other infections that are passed through genital fluids, for STIs that can be transmitted through skin contact, that's another story. "There are STIs spread through skin-to-skin contact that create visible lesions or warts," OB/GYN Felice Gersh tells Healthline. "But there are also STIs spread through skin-to-skin contact that are totally invisible to the person who has it, and their sex partner(s)."
What are those STIs? HPV and symptoms associated with HPV like genital warts, genital herpes, syphilis, and trichomoniasis. The reason for this is that condoms only cover the penis, therefore preventing the transmission of fluids (as long as the condom doesn't break or have any tears), and don't cover anything else. So when two pubic areas come in contact, then that right there is an opportunity to spread these STIs that defy condom use.
However, this doesn't mean you should ditch using condoms. Buying condoms and always having them on you so you're prepared isn't just about safe sex, but empowerment. It's just important that, when it comes to discussing the transmission and contracting of STIs, we all pay attention to the language being used, because "prevents" and "reduces risks" are two totally different things.
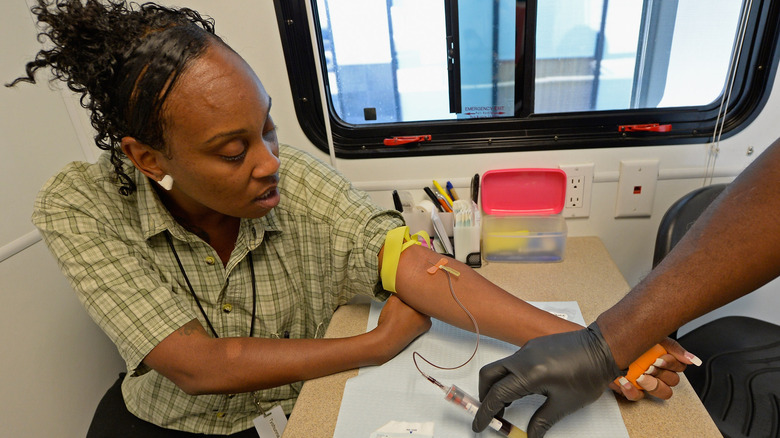
Not every STI is tested for in the same way
It makes sense that not every STI is treated the same way because of how it affects the body. But what some people don't know is that STI tests are designed for each infection. In other words, you can't roll into a clinic, pee in a cup, and assume that's all it takes.
While urine tests can be used to detect trichomoniasis and occasionally gonorrhea, these are the only two that can be accurately tested in this way. HIV, syphilis, and herpes can require blood tests, while HPV, chlamydia, gonorrhea, and herpes are diagnosed with a swab test (via Medline Plus). Although it should be noted that herpes isn't always easy to test for, and the most accurate results come from swabbing blisters during an outbreak.
In rare cases where you may possibly have advanced stages of syphilis or herpes, a spinal tap is necessary to confirm that these infections have been in the body for an extended period of time. Again, this is a rarity, so don't concern yourself with that. Instead, concern yourself with getting regular STI screenings.
Every sexually active person should get tested regularly
What's considered "regular" depends on your sexual lifestyle. If you're sexually active with multiple partners, the CDC recommends every three to six months. If you've had sex with someone, whether protected or not, and they tell you they have an STI, get tested. If you're exhibiting symptoms that make you suspicious, get tested. If you have a bad feeling and have convinced yourself you have an STI (we've all been there), then get tested so you can sleep at night. And, yes, if you're in a monogamous relationship, get tested once a year. This isn't to suggest there's any cheating happening. But research has found that in addition to many STIs not having any visible symptoms, it can sometimes take months or even years for them to appear.
If you love and respect your partner, you really have nothing to lose by getting tested — especially if the relationship is relatively new and neither of you got tested before you decided to get serious. If you intend on practicing fluid bonding, you owe it to each other to get tested. Lastly, if you've never been tested and you've had sex even once, then get yourself tested. You may not have symptoms, but that doesn't mean you won't run into the long-term effects that some STIs can have on your body, including your reproductive organs.
Your STI status isn't 'clean'
Despite the fact that STIs are profoundly common — we're in an epidemic, after all — the stigma surrounding STIs persists. What contributes to this is the language some people use when talking about their STI status. Even though no one says they're "dirty" when they're STI-positive, the mentality is there because people continue to say they're "clean" when their status is negative. If you don't have an STI, good for you. But creating a dichotomy of clean versus dirty is suggesting one is good and one is bad when that couldn't be further from the truth.
According to the Centers for Disease Control, one in five people in the US have an STI — that's 20% of the population. According to the World Health Organization, more than one million STIs are contracted every day. HPV, the most common STI, is so prevalent that the CDC has reported that just about every sexually active person will contract it at some point in their lifetime if they're not vaccinated.
People who enjoy sex and embrace their sexuality run the risk of contracting an STI. If you get one, sure, it's an inconvenience, but it's not the end of the world, not the end of your sex life, and certainly nothing of which anyone should feel ashamed. It's the stigma associated with STIs that needs to be put at the top of the list of things to cover when it comes to educating people about sexual health. When people understand that STIs are extremely prevalent and there's nothing "dirty" about them, we will have made the first step forward in re-educating people about sex and all its variables.